Benefits decision support refers to the tools and resources that help employees navigate and select the most appropriate benefits options for their individual needs. As the benefits landscape becomes more complex, employees must make critical choices about their health, financial wellness and other aspects of their lives. Effective decision support is a key part in helping participants in the moments that matter and improving employee experience.
Benefits decision support
- Empowers employees to make informed benefits choices
- Enhances overall employee satisfaction and wellbeing
- Improves utilization of benefits and aligns with organizational goals
- Reduces the complexity of benefits decisions, making the process more intuitive
Organizations that implement robust decision support systems empower their employees to make informed choices and foster a more engaged workforce. Additionally companies must shift to a new model of benefits management that provides better experiences their employees will love and greater efficiency their business needs.
With the relationship between work and life closer than ever, employers are innovating to create benefits experiences that support their wellbeing strategies and meet the unique needs of employees.
Below are some examples of how companies are elevating the employee experience with employee benefits guidance.
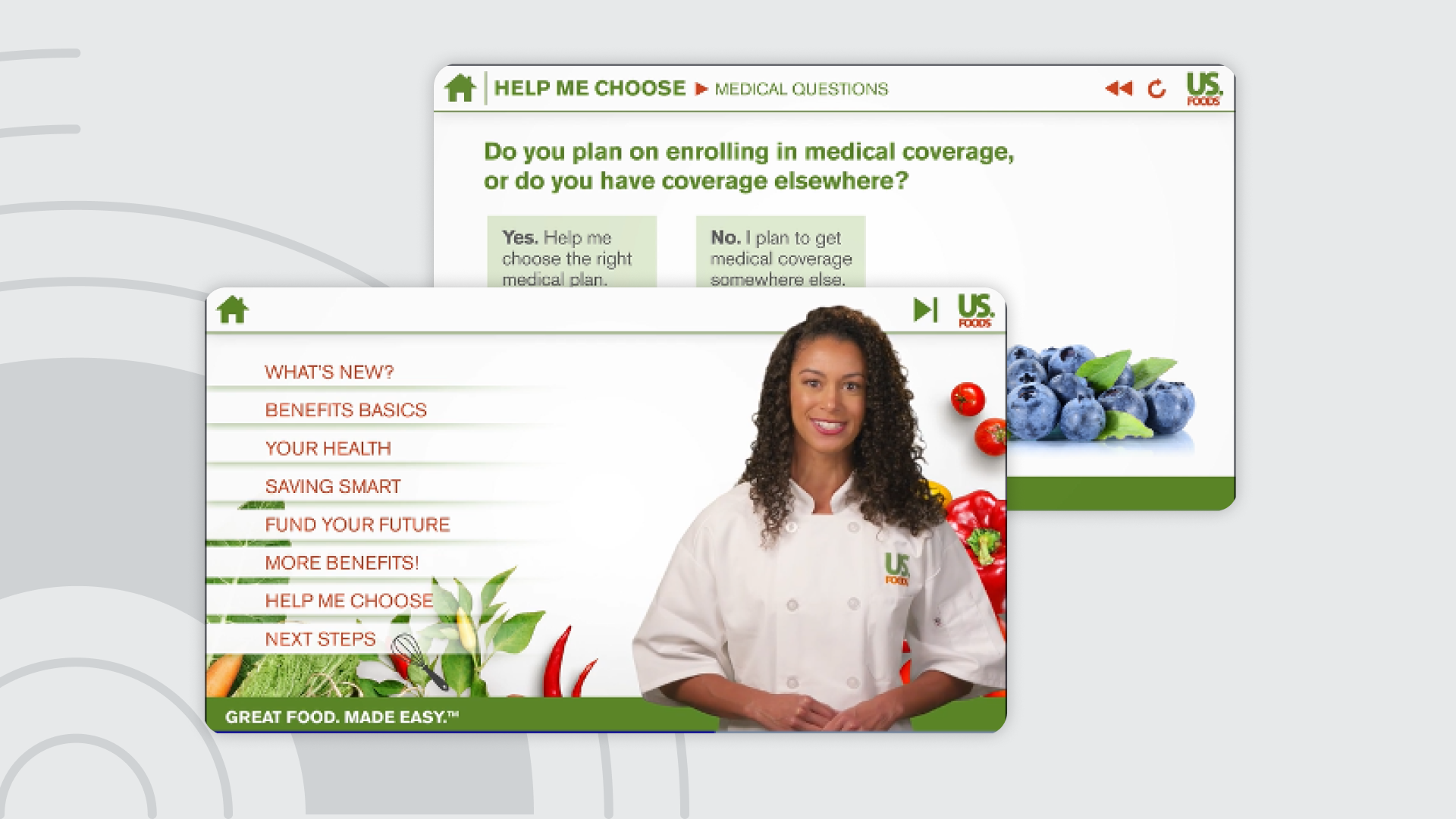
US Foods — Guided experiences for higher employee engagement
US Foods, one of America's leading food distributors, was looking for an improved and integrated way to provide benefits information to employees. With Alight’s guided experience tool, they:
- Provide associates with basic enrollment and benefits education.
- Leverage Alight Worklife® data to tailor content specific to employee groups.
- Incorporate a DecisionDirect™ tool to provide employees medical, dental and vision recommendations.
So far, the results have been quite impressive, with…
Average session duration
The final product was a grand slam! Our associates loved Chef Sage and the new experience. One of the highest engagements and the least amount of noise we ever had for an Annual Enrollment.
Health & Welfare, US Foods

Technology company — A superior benefits website for superior employee experiences
A technology company wanted a superior global website to elevate the benefits experience for their employees. They desired better navigation and organization of key information to fully promote and provide benefits guidance for the vast suite of program offerings.
Key objectives:
Interactions are simple, intuitive and straightforward
Key audiences have what they need to make good decisions
The experience is distinctive and meaningful
Key audiences trust the information and expertise received
Alight created a global website to address the needs of employees, new hires, family members and candidates from around the world. The content has been curated with an overall focus on wellbeing and moments that matter and is fully equipped with content editing capabilities.
In just over six months, the analytics reflect the following:
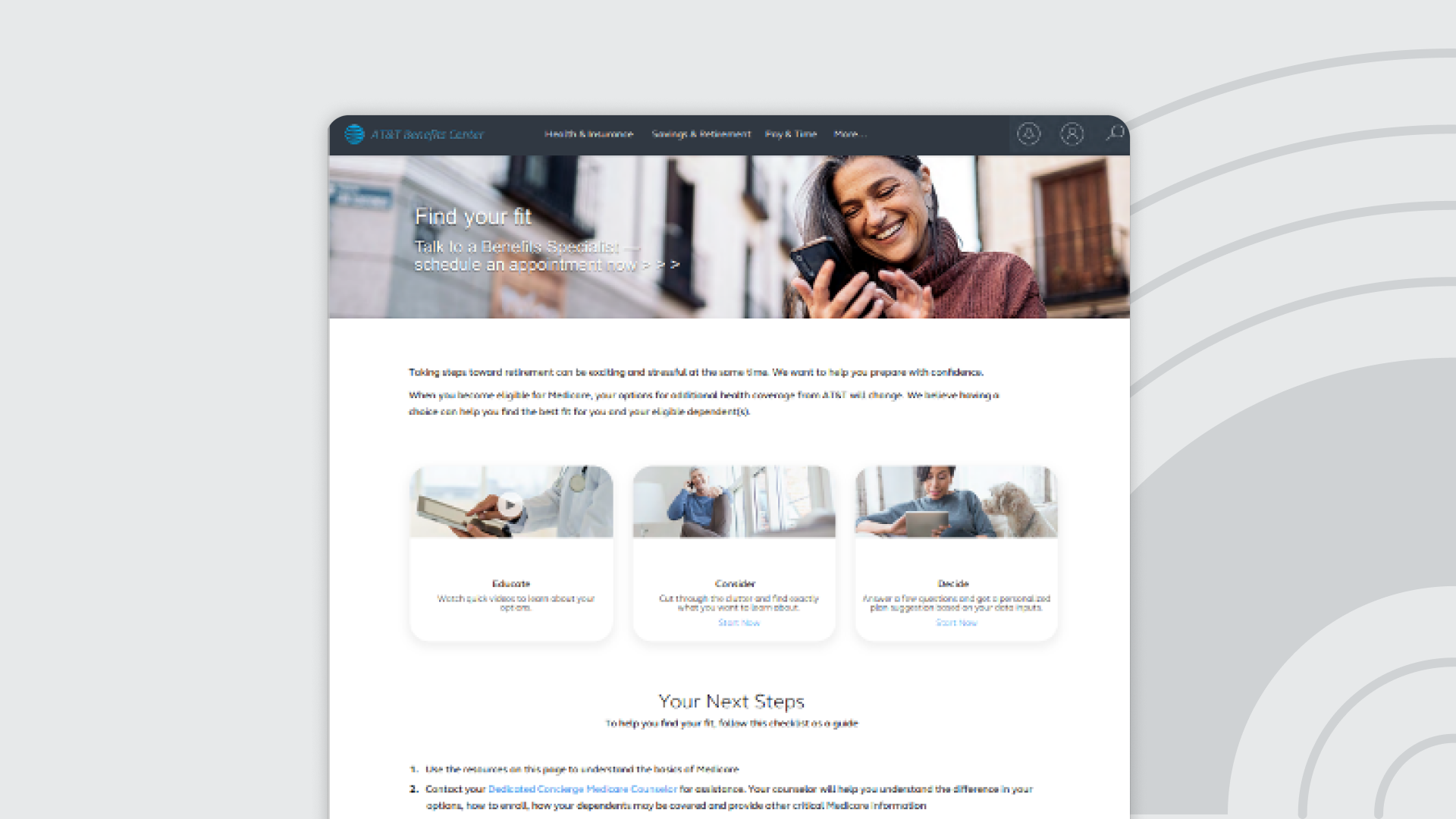
Telecommunications company — A tailored and all-inclusive employee experience
A telecommunications company wanted to help employees understand benefit options while also providing an integrated approach that addressed their specific situation. Alight crafted a simple, all-inclusive experience tailored to the participant’s needs. The all-inclusive experience started with a Medicare Advantage Prescription Drug contracting (MAPD) landing page created in Alight Worklife. The page served up links to a Guided Benefits Experience (Educate), a custom compare tool (Consider) and a DecisionDirect™ (Decide) tool to help retirees make the best decision.
Employees say it best
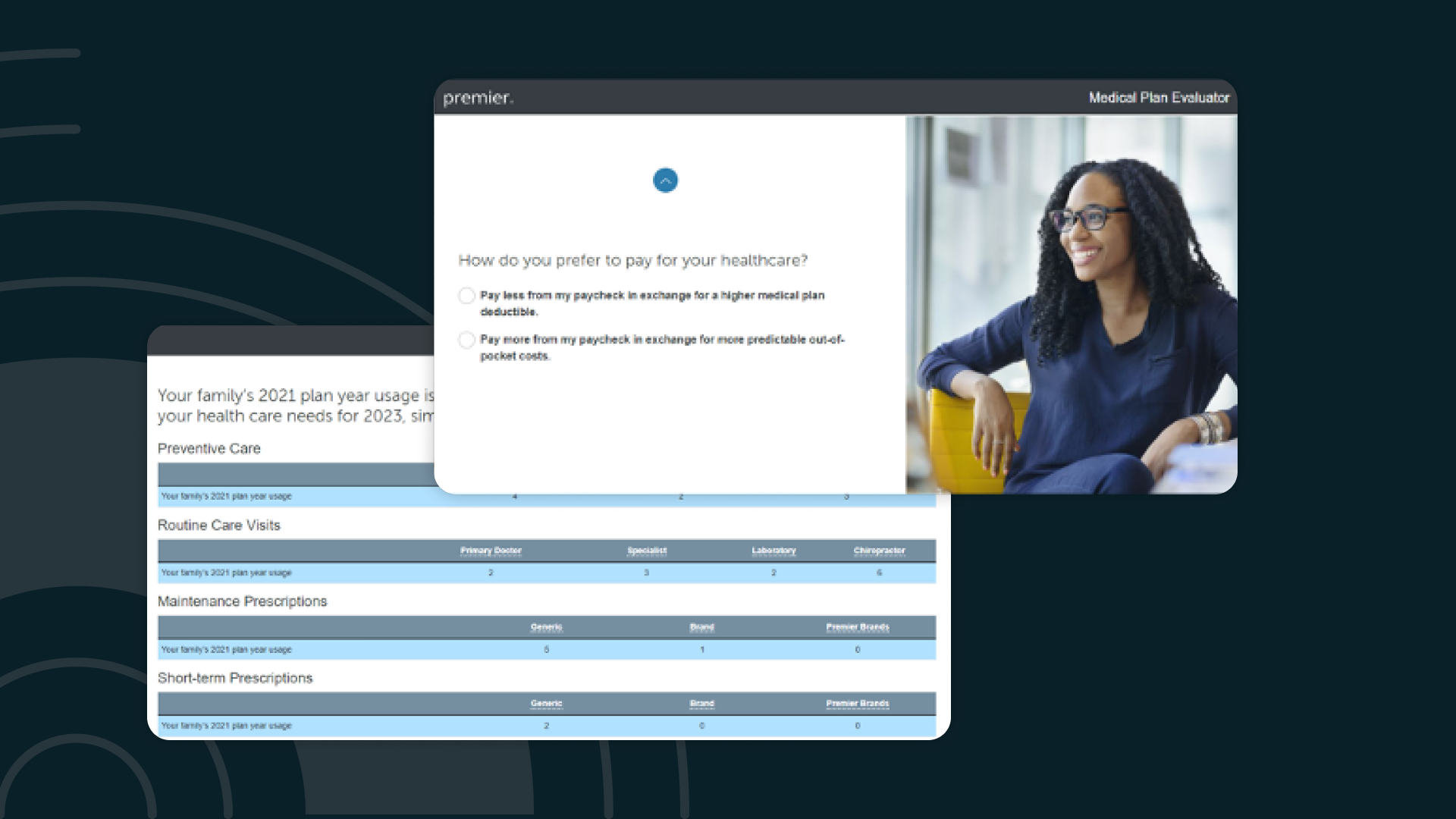
Transportation company - The right benefits coverage at the right price point
A transportation company was concerned that many of their employees were over-insured in their medical plan. They wanted an intuitive tool to help employees get the coverage they need at the right price point. They turned to Alight to help create a personalized benefits plan recommendation that makes a clear connection between cost and need. The recommendation points out when an employee’s preferences align with a lower-cost plan.
The Medical Plan Evaluator estimates out-of-pocket and total medical costs based on the employee’s actual prior usage (or national averages, if not available). Then, a proprietary algorithm weighs the cost against how the employee says they like to pay for and consume healthcare services.
The plan evaluator tool was extremely effective, with…
Users with a tendency to over-insure who were suggested a lower-cost plan
Educate, engage and drive better outcomes with Alight's Benefits Decision Support solutions: