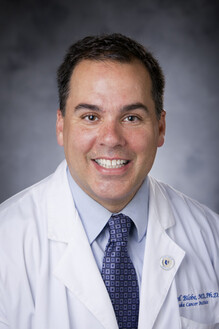
Alight recently sat down with Dr. Gerry Blobe, a leading oncologist and physician leader on Alight’s Medical Ally team, to help demystify precision medicine and its promising approach to both cancer prevention and early detection — which continues to be a top pain point for employers, per the Business Group on Health’s (BGH) 2025 Large Employer Healthcare Strategy Survey.
In addition to serving as a physician leader with Alight’s Medical Ally team, Dr. Gerry Blobe is the Professor of Medicine, Pharmacology and Cancer Biology at Duke University where he investigates new strategies for targeting cancer pathways and specializes in the treatments of colorectal and pancreatic cancer.
In this two-part series, Alight partners with Dr. Gerry Blobe to uncover the latest in precision medicine for cancer prevention and detection. In another post, we will discuss precision medicine for cancer treatment with Dr. John Strickler — a Medical Oncologist at Duke and colleague of Dr. Blobe.
Combined, the series serves to share ways that employers can unlock value and opportunity from these innovations.
(This interview was edited for clarity.)
Alight: Thanks for spending some time with us today, Dr. Blobe. Could you share a little about what precision medicine is and how it relates to cancer prevention and early detection?
Dr. Blobe: We’ve known for a long time that there’s no routine cancer. There are several things that happen to a cell that make it cancerous; certain things get turned on and others get turned off, and precision medicine sheds light on those variables. Further, it allows us to match specific therapies to what is turned on and off within a cell. In other words, we’re no longer treating every breast cancer the same, for example. The overarching goal of precision medicine for cancer prevention is to shift away from disease reaction and bring fresh impetus to early detection. Visibility into premalignancies is being revolutionized by these sequencing-based, genetic tests.
Alight: In terms of precision medicine, what are some examples of tests that are already on the market that benefits leaders might be familiar with?
Dr. Blobe: Cologuard by Exact Sciences is an at-home colon-cancer screening test that many people are already familiar with and are using to detect microscopic blood and altered DNA within the stool. Another is the Galleri multi-cancer detection test, which screens for over 50 types of cancer with a single drop of blood. Genetron Health also has a cell-free DNA blood test that is being used by Hepatitis C patients to detect early liver cancer. These are a few tests that are currently available, with many more in trial phases or early development.

Alight: When it comes to precision medicine for early cancer detection, how should we approach testing? Do you think everyone should be tested, or only those at increased risk due to age or family history?
Dr. Blobe: I think from where things stand right now, these tests should be targeted to those who are at increased risk of cancer, not the general population. For employers looking to incorporate these tests into their benefits design, that means using risk profiles to determine who should receive the tests.
Alight: Another question we have is about multi-cancer early detection tests vs. single-cancer testing. Do you recommend one over the other?
Dr. Blobe: I would lean towards more personalized and individualized testing based on a patient's family history, as opposed to multi-cancer early detection.
The multi-cancer tests are currently marketing ahead of the actual data to show future benefit to patients. But studies on many of the multi-cancer tests are currently ongoing, so we're likely going to answer this question differently in the next couple of years.
In the absence of complete data, presently, we don’t know if the multi-cancer early detection tests are going to give patients more time or cause them more stress and harm without any benefit.
Alight: Here’s a big question related to the last one: What happens if someone tests positive for cancer using these tests, and no cancer is identified in further diagnostics?
Dr. Blobe: That is one of my biggest concerns. We don't know if a positive result indicated by these early screening tests means you have cancer. A lot of precancerous cells can cause mutation, but often our immune system eliminates these cells, or they die on their own because they don't have the right order of changes to turn into cancer.
Right now, it’s possible that you could detect something that’s not going to turn into cancer. Or you might detect a cancer that’s slowly percolating but dormant — it may not cause you problems for 10, 15 or 20 years.
So now you've really stressed someone out over some potential cancer that may never affect them..
Alight: Can you speak to cancer reoccurrence testing? Is this the same technology?
Dr. Blobe: Signatera, the test we’re using in clinical practice to identify cancer relapse and monitor response to therapy, uses the same technology. It basically looks for circulating tumor DNA in the bloodstream in the same way many of the new early detection tests look for alterations in DNA or cancer cells in the blood.
Alight: What are the first steps employers can take in moving forward with precision medicine for cancer as part of their benefits design?
Dr. Blobe: In the short term of the next couple of years, employers can really help their employees by educating them first about the risks of diving into new medical technology without understanding what the negative consequences could look like.
Data and science still have some catching up to do to support the role of these tests. As we discussed, there are risks and benefits to these tests; it’s important to paint a clear picture of current limitations while sharing hope for what the future of precision medicine holds.
(End of interview.)
We want to thank Dr. Blobe for sharing his insights on precision medicine for cancer prevention and the important work his team does with us.
As a benefits leader, you can improve outcomes and support cancer prevention and early detection by:
1) Helping your employees get access to trusted resources with the latest information on precision medicine, as it relates to their health history and risk profile, in advance of full adoption, mitigating some of the risks Dr. Blobe outlined.
2) Focusing on implementing solutions that enhance healthcare literacy in the workplace. Even if you decide not to adopt a global policy on precision medicine for prevention, participants will eventually face these options with their primary care doctors or specialists. The BGH has a good roadmap that illustrates the possible gaps on the journey.
3) Continue to double-down on the actions your employees can take at this time to prevent cancer and boost health — tobacco cessation, regular exercise, proper sun protection, alcohol reduction, and getting recommended screenings based on age and risk; these are the things that drive wellness and have a substantial positive impact on employees.
4) Finally, invest time in understanding how precision medicine is addressed in your health plan and benefits strategy today. At least a quarter of employers surveyed by BGH didn’t know what tests were actually covered, presenting an opportunity to be on the front foot in promoting quality and more personalized care as innovations occur.


