In the U.S., so much of the focus on healthcare is on clinical care.
Yet food insecurity, literacy skills, safe transportation, and the various social determinants of health (SDoH) account for 80 to 90 percent of the modifiable contributors that are linked to health and risk outcomes.
In fact, a 2019 study in the journal JAMA Network Open found that social factors increased the risk of developing chronic diseases including hypertension and type-2 diabetes.
Factors like geography can also affect access to healthcare.
A recent article in Health Affairs found in rural areas with a high representation of Black or American Indian/Alaska Native populations, people were significantly farther from healthcare services than in areas with white populations.
Although SDoH have traditionally been an area of focus for Medicare and Medicaid populations, they increasingly are becoming prevalent in the commercial market and employer space.
A 2021 study in the Journal of Primary Care and Community Health, which looked at a commercially-insured population, found the following were significant barriers to care:
- cost
- family
- school
- work responsibilities
Fortunately, employer-sponsored programs or benefits that address these SDoH barriers could help, the same study found.
As employers continue to look for ways to improve their employees’ health, wellbeing, and performance at work, as well as recruit and retain top talent, addressing SDoH is vital, yet not without challenges.
In fact, a recent report by the Northeast Business Group on Health found that while employers have invested a significant amount of money in solutions such as wellness programs, digital health, and centers of excellence programs, few of these solutions have effectively addressed the SDoH.

“New” social determinants of health are coming to light
While healthcare access and equity, education, and economic stability are social determinants of health that are commonly talked about, there are other, nuanced factors we should pay attention to.
Trust in the healthcare system is one.
According to a recent report by Edelman, people with lower trust levels in the health ecosystem are less likely to engage in preventative care than those with higher trust levels—at a rate of 47% vs. 66% respectively.
The digital divide, including a lack of access to telehealth, poor broadband, and poor digital health literacy has also emerged as a social determinant of health.
“While healthcare access and equity, education, and economic stability are social determinants of health that are commonly talked about, there are other, nuanced factors we should pay attention to.”
Physicians know it’s important to address SDoH, but find it difficult to do so
Providers are well aware that addressing SDoH are vital to improving health outcomes but find it difficult to overcome the numerous obstacles.
According to a recent survey by The Physicians Foundation, 99% of physicians said that at least one SDoH affected the health outcomes of all or some their patients and 80% said that doing so is essential to improve health outcomes and decrease costs.
Yet physicians cited multiple obstacles including:
- short office visits (89%)
- lack of staff (84%)
- lack of community resources or challenges accessing them (77%)
80% physicians say addressing SDoH is essential to improve health outcomes and decrease costs
Another obstacle is that patients may not always feel comfortable having an open dialogue with their providers about social factors because they feel intimidated or embarrassed, or because their native language is a barrier.
In fact, a 2021 study in the journal Health Affairs found that due to language barriers, 25 million Spanish speakers receive about a third less healthcare than English speakers.
What’s more, they had fewer outpatient, emergency department visits, and inpatient days, and received fewer medications than Hispanic adults who speak English.
Cultural differences, racial discrimination, and implicit bias can also be a barrier to healthcare access.
25M Spanish speakers receive 1/3 less healthcare than English speakers
According to a 2021 report from the Urban Institute and the Robert Wood Johnson:
- 7.7% of Black adults and 5.2 percent of Hispanic/Latinx adults reported being treated or judged unfairly because of their race or ethnicity in the past 12 months.
Of those:
- 39% delayed care
- 30.7% didn’t get the care they needed
- 11.4% didn’t follow the provider’s recommendations
7.7% of Black adults and 5.2% of Hispanic/Latinx adults reported being treated or judged unfairly because of their race or ethnicity in the past 12 months.
What employers need to know about the social determinants of health
To properly address SDoH, awareness and education on the provider and employer sides are necessary.
We’re seeing primary care practices take a multidisciplinary team approach that includes a case manager, social worker, and behavioral health specialists to work with patients.
While providers won’t have insight into behavioral health programs or point solutions a patient may have, they should, however, have an awareness that they may be available.
Likewise, more awareness and education around SDoH is important for employers who are continually looking for ways to improve health outcomes, lower healthcare costs, and support their employees.
For example, employers may not think food insecurity is a problem for their employees, with only 1% offering healthy food programs, but work status doesn’t necessarily equate to enough food, particularly for underserved populations.

In fact, recent data shows 20% of Black and 16% of Hispanic households reported they sometimes or often did not have enough food in the past 7 days.
Employers need to be asking the tough questions to understand the needs of their employee populations and look at the programs they may have in place or need to implement.
Although there are several solutions to address food insecurity like Geisinger’s Fresh Food Farmacy and NourishedRX for example, much of this effort has been focused on Medicare and Medicaid populations.
Therefore, just as employers offer a wellbeing benefit, a solution to address food insecurity is needed.
20% of Black and 16% of Hispanic households reported they sometimes or often did not have enough food in the past 7 days.
Employers should also look at how they are targeting and motivating employees.
They may have campaigns and incentives, for example, but the messaging and the channel may not be targeted for a specific subset of the employee population and sufficient to drive change.
To address this, some employers have an on-site nurse to address healthcare literacy, identify social determinants, and guide employees to the right solution.
"Employers need to be asking the tough questions to understand the needs of their employee populations and look at the programs they may have in place or need to implement."
Healthcare Navigation & social determinants of health solutions
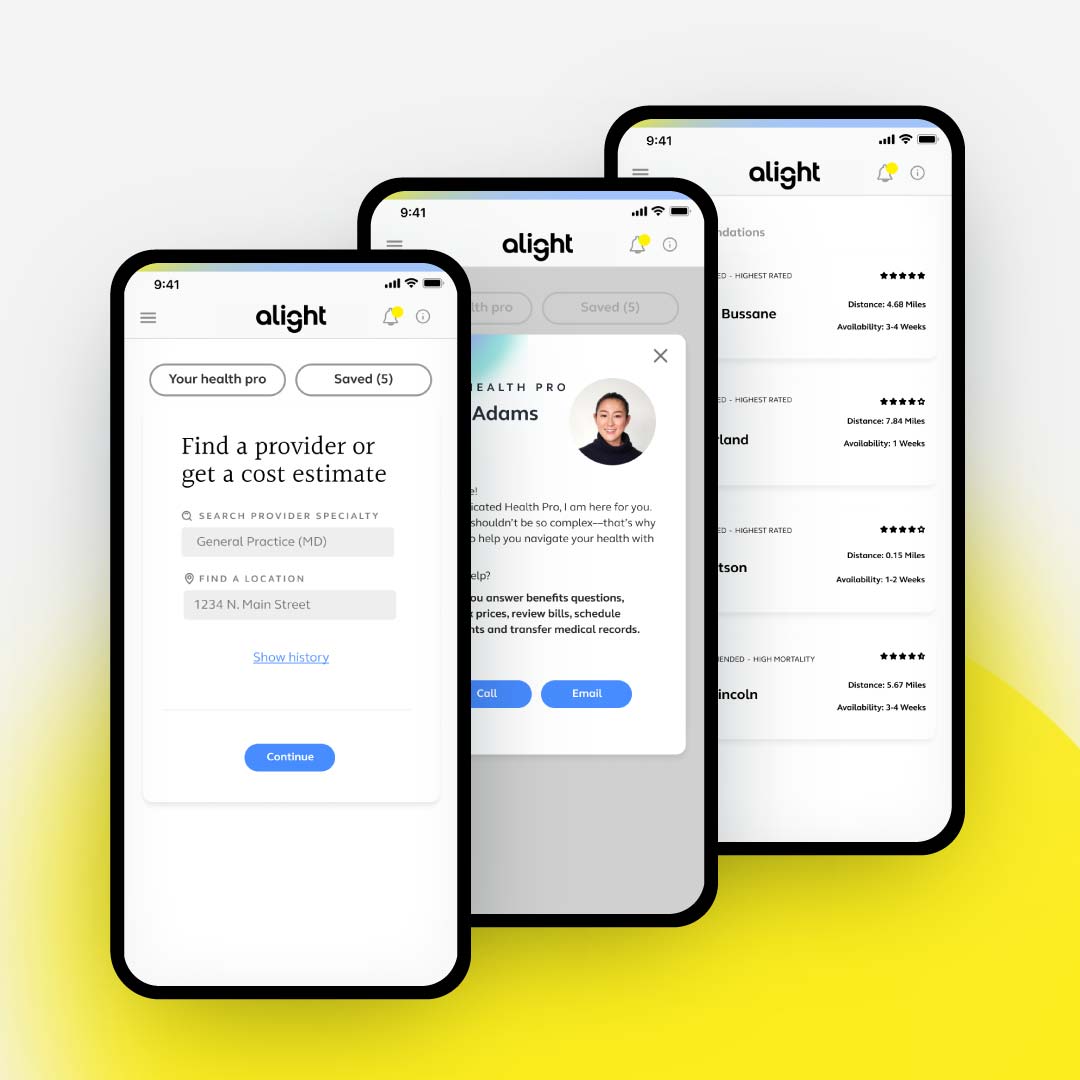
With Alight Total Guidance, and our quality provider algorithms, we can guide underserved populations to high-quality, low-cost providers, provide medical decision support to improve health literacy, and better understand their care options so they can feel better prepared for their provider visits.
We also address the social drivers based on the 5 social determinants of health domains and guide employees to appropriate solutions.